Contact Hours: 6
This online independent study activity is credited for 6 contact hours at completion.
Course Purpose
To provide healthcare professionals with an overview of suicide and assessment tools currently used to identify depression and suicide risk, common medications, and psychotherapies.
Overview
Suicide is the 10th leading cause of death in the United States. Often, healthcare professionals assess for suicide risk, but frequently, there is no follow-up or treatment instituted in someone who may be at risk. This independent study described depression and other psychiatric disorders, their influence in suicidal behavior, factors that require special intervention, major questions to ask a potentially suicidal individual, details the steps to ensure the patient’s safety, and concludes with steps that should be addressed with the family and friends in the case of a completed suicide.
Objectives
Upon completion of the independent study, the learner will be able to:
- Describe risk factors for Suicide
- Review the various types of depression
- Review the recommended tools to assess for depression and suicidal ideation
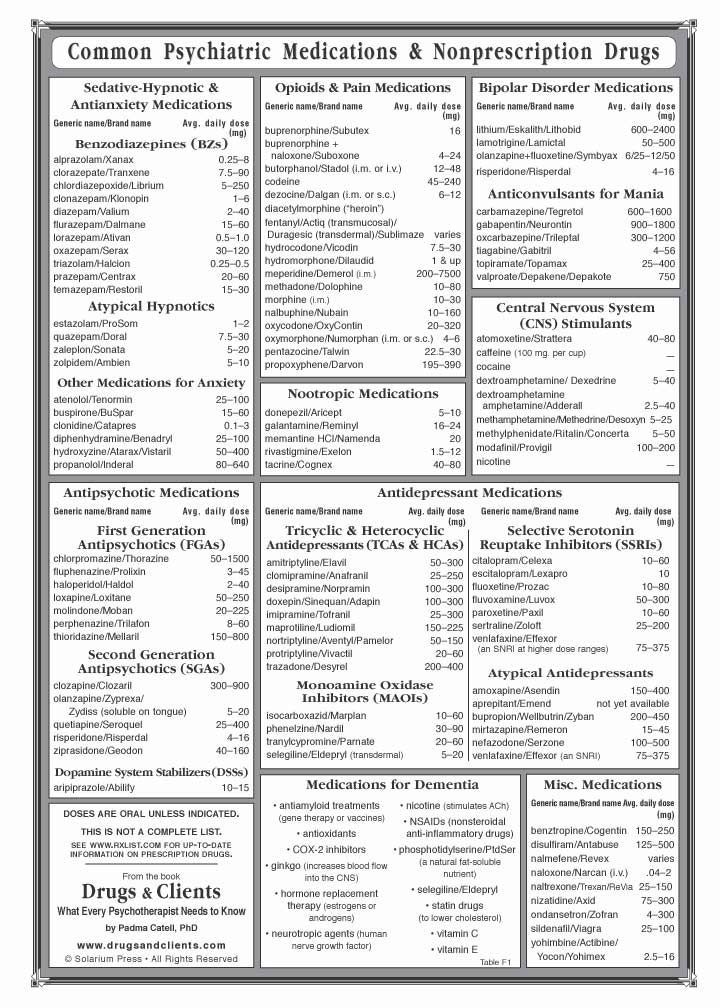
- Understand the various medications classifications used to treat depression and psychotic episodes
- Describe the steps to ensure the safety of an individual who is suicidal
Policy Statement
This activity has been planned and implemented in accordance with the policies of FastCEForLess.com. If you want to review our policy, click here.
Disclosures
Fast CE For Less, Inc. and its authors have no disclosures. There is no commercial support.
To access Fast Facts, purchase this course or a Full Access Pass.
If you already have an account, please sign in here.
To access Fast Facts, purchase this course or a Full Access Pass.
If you already have an account, please sign in here.
| Suicide | Death caused by self-directed injurious behavior with intent to die because of the behavior. |
| Suicide Attempt | A non-fatal, self-directed, potentially injurious behavior with intent to die because of the behavior. A suicide attempt might not result in injury. |
| Suicidal Ideation | Thinking about, considering, or planning suicide. |
Suicide is a major public health problem. In the United States it is the 10th leading cause of death, accounting for nearly 44,000 deaths each year. Suicide is also the seventh leading cause of years of potential loss of life, surpassing liver disease, diabetes, and HIV. Men are nearly 3.5 times more likely than women to commit suicide, and on average, 123 people kill themselves every day.
Nearly 1 out of every 7 young adults admits to having some type of suicidal ideation at some point in their lives and at least 5% have made a suicide attempt. Each year, approximately 500,000 people are treated in emergency rooms following attempted suicide. ¹˒²˒⁶
The World Health Organization (WHO) has predicted that in the next 2 years, depression will be one of the leading causes of disability globally. Depression is not only an American phenomenon; it is now being diagnosed in almost every nation. Depression is a serious medical disorder and associated with a high risk of suicide. Data reveals that more than 90% of people with major depressive disorder have seen a healthcare provider within the previous 12 months of a depressive episode and at least 45% of suicide victims have had some contact with a healthcare provider within the previous four weeks of suicide. These grim statistics have led to a National Strategy for Suicide Prevention in the United States.
Because many individuals who have committed suicide have also had a mental health disorder and had a recent visit with their healthcare provider, it is imperative for healthcare providers to become aware of the factors that increase the risk of suicide and to refer individuals to the appropriate mental health professionals.³˒⁵
Suicide Risks in Males
In recent years, there has been a steady increase in the numbers of men who have ended their life by committing suicide. While women tend to experience more suicidal thoughts, men are far more likely to die by suicide, possibly because of the increased likelihood that a male will use lethal methods such as guns when attempting suicide.⁴ The suicide rate is highest among middle-aged white men, and men over the age of 65 are at the highest risk for attempting suicide due to the following causes²⁷:
- A history of physical or sexual abuse
- Being bullied at school, college, or work
- Divorce or relationship breakdowns
- Imprisonment
- Loss of a loved one through trauma or disease
- Mental illness
- Not being able to form or sustain meaningful relationships
- Social isolation or living alone
- Unemployment
- Using drugs and/or alcohol to help cope with issues
In older men, suicide is most strongly associated with depression, physical pain, and illness, living alone, and feelings of hopelessness and guilt. In addition to the above risk factors, there are some other thoughts as to why men are at a greater risk of suicide. ¹⁷ These ideas include:
- Having a lack of emotional expression in traditional male gender roles
- This results from men being told that emotion affects masculinity and that seeking help is a sign of weakness. Having rigid gender norms may make it difficult for men to get support when they need it.
- The underdiagnosis of depression in men
- Often, men may not speak about feelings of depression to healthcare providers. Instead, they may describe feeling stressed regarding issues at work rather than describe feeling sad or hopeless.
- Lack of assistance for mental health
- Research has suggested that mental health diagnoses such as depression are less frequently diagnosed in men. This may result from tendencies to deny mental illness, choosing to self-monitor symptoms, and self-treat or self-medicate with alcohol or other substances.
Suicide Risks in Pregnancy
Even though postpartum depression is commonly reported in women, the actual rates of suicide are rare. Suicide during pregnancy is even rarer. In any case, pregnant and postpartum females should be screened for depression. ²⁸
Suicide Risks in the Military
Historically, military suicide rates have been lower than rates within the general population, however, there has been a rise in the suicide rates within the military veterans over the past 10 years.¹⁵ Currently, suicide is the second leading cause of death in the military. According to the Department of Defense Suicide Event Report (DoDSER) annual report, the standardized suicide rate was 20 per 100,000 for the active military members, 24 per 100,000 for members of the reserve, and 27 per 100,000 for members of the national guard. There are several factors that are associated with the increased suicide risk, including:
- Relationship problems
- Administrative/legal issues
- Workplace difficulties
- Traumatic brain injury (TBI)
- Chronic pain
- Sleep disorders.
- Post-Traumatic Stress Disorder (PTSD)
- Other mental health issues
The above conditions have been found to contribute substantially to the increased suicide risk among military members. According to the DODSER annual report, the most common method for suicide is firearms, which accounts for over 60% of all suicide deaths in the military.
The risk for suicide does not decline once an individual completes military service. Military veterans have a much greater risk for suicide than the average civilian. According to the Office of Suicide Prevention, military veterans account for approximately 18% of all adult suicide deaths in the United States, even though veterans only make up approximately 9% of the population. This means that approximately 20 military veterans die each day by suicide, which highlights the disproportionate number of suicide deaths among this group0.¹⁵ Like active military and service members, the most common method for suicide among military veterans is firearms, accounting for over 66% of all veteran suicides.
With the significant increased suicide rates in our military population, it is imperative that we provide evidence-based psychotherapies developed specifically to target suicidal thoughts and behaviors. Cognitive Therapy for Suicide Prevention (CT-SP) is an evidence-based treatment recommended by the VA/DOD Clinical Practice Guideline for the Assessment and Management of Patient’s at Risk for Suicide. CT-SP is a structured, time-limited, present-focused approach that helps patients develop coping skills and strategies to overcome suicidal crises.
The most important thing to understand is that having just one risk factor has extremely limited predictive value. Millions of Americans have one of these factors at any one point in time, but very few attempt suicide and even fewer die as a result. One must look at the entire clinical picture to increase the predictive values of these risk factors.
In the United States, the most common method of committing suicide is with the use of firearms. On average, approximately 50% of people who commit suicide will use a gun. Men more likely to use a firearm compared to women, as 56% who commit suicide will use a gun, compared to only 30% of women.⁴ Furthermore, the risk of suicide with a firearm in men increases when the depressed individual also uses alcohol. Other causes of suicide include the use of medications, jumping off buildings, hanging, jumping in front of a train, suffocation, poisoning, or drowning.
All healthcare workers should be aware of the state statutes on possession of firearms and mental illness. Many states ban the possession of firearms by individuals with mental illness, but recent shootings in the United States indicate that many mentally ill patients continue to have access to guns. ⁴
Mental health includes emotional, psychological, and social well-being. It affects how one thinks, feels, and acts, and helps determine how stress is managed. Mental illnesses are conditions that affect one’s behavior, feeling, mood, or thinking. Mental illnesses are among the most common health conditions in the United States. Statistically, more than 50% of the population will be diagnosed with a mental illness or disorder at some point in their lifetime.⁷ Also, within a 12 month period, 20% of the population will experience mental illness and 4% of the population will have a debilitating mental illness.
Although the terms are often used synonymously, poor mental health and mental illness are not the same things. One can experience poor mental health and not be diagnosed with a mental illness. Similarly, one who is diagnosed with a mental illness can experience periods of mental well-being.
There are many types of mental health disorders that have been associated with an increased risk of suicide. They include the following:
Major Depression
Major depression is more than just a passing blue mood, a bad day, or temporary sadness. The symptoms of major depression are defined as lasting at least two weeks or more and may occur once, or repeatedly over one’s life. During a major depressive episode, thinking can become obscured. People with major depression may also experience patterns of high or low energy, or irritability. ⁷˒¹⁶ The severe form of major depression is called mania or having a manic episode. One who has milder symptoms of mania and does not experience delusional behavior is said to have hypomania, or a hypomanic episode. Symptoms of major depression include:
- Appearing slowed or agitated
- Decreased or increased sleep
- Decreased or increased weight or appetite
- Distinctly depressed or irritable mood
- Fatigue and loss of energy
- Feeling worthless or guilty
- Loss of interest or pleasure
- Poor concentration or indecisiveness
- Thoughts of death, suicide attempts or plans
Another form of major depression can occur within the first 3 months of giving birth to a baby. This form of depression is called postpartum depression. It is different from baby blues, which occurs within 3 days after childbirth and can last two weeks. The symptoms of baby blues include mood swings, crying spells, anxiety and difficulty sleeping. Initially, postpartum depression may be mistaken for baby blues, however the symptoms of postpartum depression are more intense and can last one year or longer. Symptoms of postpartum depression include:
- Depressed mood or severe mood swings
- Difficulty bonding with your baby
- Diminished ability to think clearly, concentrate or make decisions
- Excessive crying
- Fear that you are not a good mother
- Feelings of worthlessness, shame, guilt, or inadequacy
- Hopelessness
- Inability to sleep (insomnia) or sleeping too much
- Intense irritability and anger
- Loss of appetite or eating much more than usual
- Overwhelming fatigue or loss of energy
- Recurrent thoughts of death or suicide
- Reduced interest and pleasure in activities you used to enjoy
- Restlessness
- Severe anxiety and panic attacks
- Thoughts of harming yourself or your baby
- Withdrawing from family and friends
In severe cases, postpartum psychosis may occur. The mother of the newborn may lose touch with reality and experience hallucinations or delusions. This severe form of major depression is rare, occurring in only 2 out of 1,000 women who experience childbirth. Most often, women who experience postpartum psychosis have a history of mental health diagnosis, including schizoaffective disorder, bipolar disorder, or experiencing postpartum psychosis in a previous pregnancy. It also can occur with a first pregnancy, or when a mother discontinues her psychiatric medications during pregnancy. Symptoms of postpartum psychosis include:
- Auditory hallucinations
- Delusional beliefs that are usually related to the infant, such as that others are trying to harm her baby
- Disoriented to place and time
- Erratic and unusual behavior
- Rapidly changing moods from extreme sadness to very energetic
- Suicidal thoughts
- Violent thoughts, such as telling a mother to hurt her baby
Another form of depression that occurs mainly during the winter months is called seasonal affective disorder, or SAD. It also may be called major depressive disorder with seasonal pattern. Seasonal affective disorder symptoms usually appear during late fall or early winter and go away during spring and summer, however, the opposite pattern of symptoms during the spring and summer that resolve during the fall and winter have been reported. In either case, symptoms may start out mild and become more severe as the season progresses. Signs and symptoms of seasonal affective disorder may include:
- Feeling depressed most of the day, nearly every day
- Losing interest in activities
- Having low energy
- Having problems with sleeping
- Experiencing changes in appetite or weight
- Feeling sluggish or agitated
- Having difficulty concentrating
- Feeling hopeless, worthless, or guilty
- Having frequent thoughts of death or suicide
It is important to note, that episodes of depression can occur at any age, and depression is diagnosed in women twice as often as in men. Also, people who have a family member with major depression are more likely to develop depression.
Schizophrenia
Schizophrenia is a serious mental illness that affects how someone behaves, feels, and thinks. People with schizophrenia may appear to have a lack of sense of reality, which can cause significant distress for people with schizophrenia, their family members, and their friends.⁸ If schizophrenia is untreated, the symptoms may persist and become disabling.
Schizophrenia is usually diagnosed in late teens to early thirties. A diagnosis of schizophrenia often follows the first episode of psychosis when symptoms are first observed. Schizophrenia can occur in younger children, but it is rare for it to occur before adolescence.
The symptoms of schizophrenia generally fall into the following three categories:
| Psychotic: | Include abnormal thinking, altered perceptions, and odd behaviors. People with psychotic symptoms may lose a sense of reality and experience the world in a distorted way. A person who is psychotic may experience: · Auditory and visual hallucinations · Delusions and paranoia · Thought disorder or disorganized speech |
| Negative: | Includes loss of motivation, lack of enjoyment in daily activities, social withdrawal, difficulty showing emotions, and difficulty functioning normally. A person with negative symptoms may experience: · Reduced motivation and difficulty with activities · Lack of happiness and satisfaction with life · Lack of expression of emotions; flat affect · Reduced speaking |
| Cognitive: | Includes problems in attention, concentration, and memory. These symptoms may be subtle for some and profound for others. A person with cognitive symptoms may experience: · Difficulty processing information to make decisions · Problems using information immediately after learning it · Trouble focusing or paying attention |
Schizophrenia sometimes runs in families, but just because an individual has a family history of schizophrenia does not mean that they themselves will have it. There are other causes that can contribute to the development of schizophrenia, like environmental factors such as poverty, lack of adequate nutrition, virus exposure, and variations in brain function and interactions among neurotransmitters. Changes to the brain that occur during puberty may trigger psychotic episodes in people who are already vulnerable to schizophrenia because of environmental exposures, genetics, or the types of brain differences that have been mentioned.
Substance Abuse
Drug addiction, also called substance use disorder, is a disease that affects one’s brain and behavior, and leads to an inability to control the use of legal or illegal drugs. Substance abuse can lead to dependency and physiological symptoms that develop after repeated substance use. The symptoms often include a strong desire to take a drug or consume alcohol, difficulties in controlling drug or alcohol use, continuing to use drugs or alcohol despite the harmful consequences, giving higher priority to the drug or alcohol than to other activities and obligations, increased tolerance, and a physical withdrawal when the drug or alcohol is stopped.
Substance abuse can start with experimental use of a recreational drug in social situations. Some people may never develop drug addiction; however, others may develop it as the drug use becomes more frequent. In other instances, especially with opioids, substance abuse can begin with taking prescribed medications or taking medications from a friend or relative who has been prescribed a medication.
Symptoms of substance abuse include:
- Continuing to use a drug even when it causes physical or psychological harm
- Driving or doing other risky activities while under the influence of a drug
- Ensuring that there is a supply of a drug
- Experiencing withdrawal symptoms when the drug is stopped
- Failing to stop using a drug independently
- Having a strong desire or urge to use a drug
- Needing to take more of a drug to get the same effect
- Not meeting personal obligations and work responsibilities
- Spending a good deal of time getting a drug, using a drug, or recovering from the effects of a drug
- Spending money on a drug, even when it cannot be afforded
- Taking larger amounts of the drug over a longer period
- Taking uncharacteristic actions such as stealing
Alcoholism
Alcoholism is also known as alcohol abuse, alcohol dependence and alcohol use disorder. Alcoholism occurs when a person drinks alcohol to the point that the body becomes dependent on it. Those who suffer from alcoholism will continue to drink alcohol even when drinking causes negative consequences, like losing a job or destroying relationships with people they love.
Although the exact cause of alcoholism is unknown, there are certain factors that may increase one’s risk for developing the disease. The factors include:
- A parent with history of alcoholism
- Consuming more than 12 drinks per week for a female
- Consuming more than 15 drinks per week for a male
- Consuming more than 5 drinks per day at least once a week; binge drinking
- Diagnosed with mental health problem
Symptoms of alcohol use disorder include:
- Being unable to limit the amount of alcohol consumption
- Continuing to drink alcohol even when it is causing physical, social, or interpersonal problems
- Developing a tolerance to alcohol where more is needed for the same effect
- Experiencing withdrawal symptoms including nausea, sweating and tremors
- Failing to fulfill major obligations at work, school, or home due to repeated alcohol use
- Feeling a strong craving or urge to drink alcohol
- Stopping social and work activities and hobbies
- Spending a lot of time getting alcohol, drinking, or recovering from alcohol use
- Using alcohol in unsafe situations, such as driving while intoxicated
- Being unable to stop the consumption of alcohol even when an individual has a desire to do so
Post-Traumatic Stress Disorder
Post-traumatic stress disorder (PTSD) is a mental health condition that occurs after seeing or experiencing a traumatic event. Not everyone with PTSD has experienced a dangerous event such as war. Some experiences like the sudden death of a loved one can also cause PTSD. Symptoms of PTSD usually begin within 3 months but sometimes they begin years after the traumatic event. ⁷ Symptoms must last more than a month and be severe enough to interfere with daily functioning to be considered PTSD. The course of PTSD varies from person to person. Some people recover within 6 months, while others have symptoms that last much longer. In some people, the condition may become chronic. Most people who experience traumatic events may have temporary difficulty adjusting and coping, but these symptoms usually last less than one month. This is termed acute stress disorder. When the symptoms get worse or last for months or years and interferes with daily functioning, it is likely PTSD.
Symptoms of post-traumatic stress disorder may include:
- Always being on guard for danger
- Avoiding places, activities or people that remind you of the traumatic event
- Being easily startled or frightened
- Difficulty experiencing positive emotions
- Difficulty maintaining close relationships
- Feeling detached from family and friends
- Feeling emotionally numb
- Hopelessness about the future
- Irritability, angry outbursts, or aggressive behavior
- Lack of interest in activities
- Memory problems, including not remembering important aspects of the traumatic event
- Negative thoughts about oneself, other people, or the world
- Overwhelming guilt or shame
- Recurrent, unwanted distressing memories of the traumatic event
- Reliving the traumatic event as if it were happening again
- Self-destructive behavior
- Severe emotional distress or physical reactions to something that reminds you of the traumatic event
- Trouble concentrating
- Trouble sleeping
- Trying to avoid thinking or talking about the traumatic event
- Upsetting dreams or nightmares about the traumatic event
Bipolar Disorder
Bipolar disorder is a mental health condition that causes extreme mood swings. The mood swings include emotional highs (mania or hypomania) and emotional lows (depression). The mood swings can occur rarely, or several times a year. ⁷
Mania and hypomania are two distinct types of episodes of bipolar disorder, but they have the same symptoms. Mania is more severe than hypomania and causes more noticeable problems in relationships and during every-day activities. Mania may also trigger a break from reality (psychosis) and require hospitalization.
Both manic and hypomanic episodes include three or more of the following symptoms:
- Abnormally upbeat
- Decreased need for sleep
- Distractibility
- Exaggerated sense of well-being and self-confidence, feeling euphoric
- Increased activity, energy, or agitation
- Poor decision-making
- Racing thoughts
- Unusual talkativeness
A major depressive episode in bipolar disorder includes symptoms that are severe enough to cause noticeable difficulty in every-day activities and relationships. An episode of depression in bipolar disorder includes five or more of the following symptoms:
There are several types of bipolar and related disorders. They may include mania or hypomania and depression. Symptoms can cause unpredictable changes in mood and behavior, resulting in significant distress and difficulty in life. Types of bipolar disorder include:
| Bipolar I Disorder: | Having at least one manic episode that may be preceded or followed by hypomanic or major depressive episodes. In some cases, mania may trigger a break from reality (psychosis). |
| Bipolar II Disorder: | Having at least one major depressive episode and at least one hypomanic episode, without having a manic episode. |
| Cyclothymic Disorder: | Having at least two years of multiple episodes of hypomania symptoms and periods of depressive symptoms without major depression. |
| Other Types: | These include bipolar and related disorders caused by drug or alcohol consumption, or due to a medical condition such as Cushing’s disease, multiple sclerosis, or stroke. |
Bipolar II disorder is not a milder form of bipolar I disorder, but a separate diagnosis. While the manic episodes of bipolar I disorder can be severe and dangerous, individuals with bipolar II disorder can be depressed for longer periods, which can cause significant impairment. Bipolar disorder can occur at any age, but it is usually diagnosed before the age of 30. Symptoms can vary from person to person, and symptoms may vary over time.
Personality Disorders
Personality disorders are defined by patterns and behaviors that differ from social norms and expectations.¹⁹ A person who is diagnosed with a personality disorder has difficulty perceiving and relating to situations and people, thinking, functioning, and behaving. Personality disorders cause problems and limitations in relationships, social activities, work, and school, and are associated with significant distress or disability. Often, a person may not realize that they have a personality disorder because they may think that their thoughts and behaviors are appropriate, may lack insight into their condition, and may refrain from seeking treatment.¹⁹ This behavior can result in maladaptive coping skills and may lead to more personal problems that cause extreme anxiety, distress, or depression, resulting in impaired psychosocial functioning. These behavior patterns usually begin in adolescence but can also be recognized in childhood and early adulthood. There are many types of personality disorders and some types may become less obvious throughout middle age.
Personality disorders with similar characteristics and symptoms are grouped into three clusters. According to the Diagnostic and Statistical Manual of Mental Disorders, fifth edition (DSM-5), a personality disorder can be diagnosed if there are significant impairments in self and interpersonal functioning and one or more pathological personality traits. Personality disorders are found on Axis II (underlying pervasive and personality conditions) of the diagnostic manual of the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders. For a person to be diagnosed with a personality disorder, they must experience the following in addition to criteria listed within a personality disorder:
- Have experiences and behaviors that are outside cultural norms in two of the following areas:
- Cognition: Perception of self and others
- Affect: Range and intensity of appropriate emotional response
- Interpersonal Functioning
- Impulse Control
- Have a pattern of behavior that is inflexible and pervasive in a broad range of personal and social situations.
- Having a long, stable behavior pattern that is initially observed in adolescence or early adulthood and is not attributed to another mental disorder.
- Having a pattern of behavior that leads to significant distress or social impairment in social or work environments.
- The behavior pattern is not the result of substance abuse or a medical condition.
DSM-5 Personality Disorders
The DSM-5 lists 10 personality disorders and groups each one into one of three clusters: A (odd or eccentric disorders), B (dramatic emotional or erratic disorders), or C (anxious or fearful disorders).
Cluster A Personality Disorders
Cluster A personality disorders are characterized by odd, eccentric thinking or behavior. They include paranoid personality disorder, schizoid personality disorder and schizotypal personality disorder.
| Paranoid Personality Disorder: | Characterized by a pattern of irrational suspicion and mistrust of others, interpreting motivations as malevolent. Individuals with this disorder may also exhibit: – Angry or hostile reaction to perceived slights or insults – Hesitancy to confide in others due to unreasonable fear that others will use the information against them – Perception of innocent remarks or non-threatening situations as personal insults or attacks – Pervasive distrust and suspicion of others and their motives – Tendency to hold grudges – Unjustified belief that others are trying to harm or deceive them – Unjustified suspicion of the loyalty or trustworthiness of others – Unjustified, recurrent suspicion that spouse or sexual partner is unfaithful |
| Schizoid Personality Disorder: | Characterized by a lack of interest and detachment from social relationships, apathy, and restricted emotional expression. Individuals with this disorder may also exhibit: – An appearance of being cold or indifferent to others – Inability to pick up normal social cuesInability to take pleasure in most activities – Lack of interest in social or personal relationships – Preferring to be alone – Limited range of emotional expression – Little or no interest in having sex with another person |
| Schizotypal Personality Disorder: | Characterized by a pattern of extreme discomfort interacting socially, and distorted cognition and perceptions. Individuals with this disorder may also exhibit: Beliefs that one can influence people and events with their thoughts – Beliefs that certain casual incidents or events have hidden messages meant only for them – Flat emotions or inappropriate emotional responses – Indifferent, inappropriate, or suspicious response to others – Auditory and visual hallucinationsPeculiar dress, thinking, beliefs, speech, or behavior – Social anxiety and difficulty with close relationships |
Cluster B Personality Disorders
Cluster B personality disorders are characterized by dramatic, overly emotional, or unpredictable thinking or behavior. They include antisocial personality disorder, borderline personality disorder, histrionic personality disorder and narcissistic personality disorder.
| Antisocial Personality Disorder: | Characterized by a pervasive pattern of disregard and violation of the rights of others, lack of empathy, bloated self-image, manipulative and impulsive behavior. Individuals with this disorder may also exhibit: – Aggressive, violent behavior – Consistently irresponsible – Disregard for others’ needs or feelings – Disregard for the safety of self or others – Impulsive behavior – Lack of remorse for behavior – Persistent lying, stealing, using aliases, conning others – Recurring problems with the law – Repeated violation of the rights of others |
| Borderline Personality Disorder: | Characterized by a pervasive pattern of abrupt mood swings, instability in relationships, self-image, identity, behavior and affect often leading to self-harm and impulsivity. Individuals with this disorder may also exhibit: – Frequent, intense displays of anger – Impulsive and risky behavior – Intense fear of being alone or abandoned – Ongoing feelings of emptiness – Stress-related paranoia that comes and goes – Suicidal behavior or threats of self-injury – Unstable and intense relationships – Unstable or fragile self-image – Up and down moods, often as a reaction to interpersonal stress |
| Narcissistic Personality Disorder: | Characterized by a pervasive pattern of grandiosity, need for admiration, and a perceived or real lack of empathy. In a more severe expression, narcissistic personality disorder may show evidence of paranoia, aggression, psychopathy, and sadistic personality disorder, which is known as malignant narcissism. Persons with this disorder may also exhibit: – Arrogance – Belief that one is special and more important than others – Having envy of others or believing that others envy them – Exaggeration of achievements or talents – Expectation of constant praise and admiration – Failure to recognize others’ needs and feelings – Fantasies about power, success, and attractiveness – Unreasonable expectations of favors and advantages, often taking advantage of others |
Cluster C Personality Disorders
Cluster C personality disorders are characterized by anxious, fearful thinking or behavior. They include avoidant personality disorder, dependent personality disorder and obsessive-compulsive personality disorder.
| Avoidant Personality Disorder: | Characterized by pervasive feelings of social inhibition and inadequacy, extreme sensitivity to negative evaluation. Persons with this disorder may also exhibit: – Too sensitive to criticism or rejection – Feeling inadequate, inferior, or unattractive – Avoidance of work activities that require interpersonal contact – Socially inhibited, timid and isolated, avoiding new activities or meeting strangers – Extreme shyness in social situations and personal relationships – Fear of disapproval, embarrassment, or ridicule |
| Dependent Personality Disorder: | Characterized by a pervasive psychological need to be cared for by other people. Persons with this disorder may also exhibit: – Difficulty disagreeing with others, fearing disapproval – Difficulty starting or doing projects independently due to lack of self-confidence – Excessive dependence on others and feeling the need to be taken care of – Fear of having to provide self-care or fend for oneself if left alone – Lack of self-confidence, requiring excessive advice and reassurance from others to make even small decisions – Submissive or clingy behavior toward others – Tolerance of poor or abusive treatment, even when other options are available – Urgent need to start a new relationship when a close one has ended |
| Obsessive-Compulsive Personality Disorder: | Characterized by rigid conformity to rules, perfectionism, and control to the point of satisfaction and exclusion of leisurely activities and friendships. Persons with this disorder may also exhibit: – Desire to be in control of people, tasks and situations, and inability to delegate tasks – Extreme perfectionism, resulting in dysfunction and distress when perfection is not achieved – Inability to discard broken or worthless objects – Inflexible about morality, ethics, or values – Neglect of friends and enjoyable activities because of excessive commitment to work or a project – Preoccupation with details, orderliness, and rules – Rigid and stubborn – Tight control over budgeting and spending money – Obsessive-compulsive personality disorder is not the same as obsessive-compulsive disorder, a type of anxiety disorder. |
Personality disorders are not only grouped by category and cluster. It is also possible to classify personality disorders using additional factors such as severity of the disorder, impact on social functioning, and attribution.
Classifying personality disorders by severity uses a subthreshold (personality difficulty) as a measure of scores for personality disorder. These scores use interviews and show evidence that people with the most severe personality disorders will likely demonstrate a ripple effect of personality disturbance across the whole range of mental disorders. This is demonstrated in the table below:
Dimensional System of Classifying Personality Disorders
| Level of Severity | Description | Definition by Categorical System |
| 0 | No Personality Disorder | Does not meet actual or subthreshold criteria for any personality disorder |
| 1 | Personality Difficulty | Meets subthreshold criteria for one or several personality disorders |
| 2 | Simple Personality Disorder | Meets actual criteria for one or more personality disorders within the same cluster |
| 3 | Complex (Diffuse) Personality Disorder | Meets actual criteria for one or more personality disorders within more than one cluster |
| 4 | Severe Personality Disorder | Meets criteria for creation of severe disruption to both individual and to many in society |
There are several advantages to classifying personality disorder by severity. For instance, it takes advantage of the tendency for personality disorders to be comorbid with each other, it shows personality disorders’ influence on clinical outcomes, and it accommodates the new diagnosis of severe personality disorder, particularly severe personality disorder.
Effect on social functioning
Social functioning is affected by many other aspects of mental functions apart from personality. Whenever social functioning is impaired when it normally would not be, it is more likely to be created by a personality abnormality than by other clinical causes. The Personality Assessment Schedule prioritizes social functioning by creating a hierarchy where a personality disorder that creates social dysfunction is most important over other personality disorders.
Attribution
Often, people who have a personality disorder do not recognize that their behaviors are abnormal and will refuse treatment. This group has been termed the Type R, or people with treatment-resisting personality disorders, as opposed to the Type S or those with treatment-seeking personality disorders. These people accept that they have a personality disorder and are active in seeking treatments for improved behaviors.
Emotional Stress
Emotional stress is a condition that occurs when a person’s emotions are affected when they are stressed. There are several contributors to stress; finances, work, family life etc. and not being able to cope with stress can produce physical and emotional symptoms. Emotional signs of stress can include:
The DSM-5 lists 10 personality disorders and groups each one into one of three clusters: A (odd or eccentric disorders), B (dramatic emotional or erratic disorders), or C (anxious or fearful disorders).
Cluster A Personality Disorders
Cluster A personality disorders are characterized by odd, eccentric thinking or behavior. They include paranoid personality disorder, schizoid personality disorder and schizotypal personality disorder.
| Paranoid Personality Disorder: | Characterized by a pattern of irrational suspicion and mistrust of others, interpreting motivations as malevolent. Individuals with this disorder may also exhibit: – Angry or hostile reaction to perceived slights or insults – Hesitancy to confide in others due to unreasonable fear that others will use the information against them – Perception of innocent remarks or non-threatening situations as personal insults or attacks – Pervasive distrust and suspicion of others and their motives – Tendency to hold grudgesUnjustified belief that others are trying to harm or deceive them – Unjustified suspicion of the loyalty or trustworthiness of others – Unjustified, recurrent suspicion that spouse or sexual partner is unfaithful |
| Schizoid Personality Disorder: | Characterized by a lack of interest and detachment from social relationships, apathy, and restricted emotional expression. Individuals with this disorder may also exhibit: – An appearance of being cold or indifferent to others – Inability to pick up normal social cuesInability to take pleasure in most activities – Lack of interest in social or personal relationshipsPreferring to be alone – Limited range of emotional expression – Little or no interest in having sex with another person |
| Schizotypal Personality Disorder: | Characterized by a pattern of extreme discomfort interacting socially, and distorted cognitions and perceptions. Individuals with this disorder may also exhibit: – Beliefs that one can influence people and events with their thoughts – Beliefs that certain casual incidents or events have hidden messages meant only for them – Flat emotions or inappropriate emotional responses – Indifferent, inappropriate, or suspicious response to others – Auditory and visual hallucinations – Peculiar dress, thinking, beliefs, speech, or behavior – Social anxiety and difficulty with close relationships |
Cluster B Personality Disorders
Cluster B personality disorders are characterized by dramatic, overly emotional, or unpredictable thinking or behavior. They include antisocial personality disorder, borderline personality disorder, histrionic personality disorder and narcissistic personality disorder.
| Antisocial Personality Disorder: | Characterized by a pervasive pattern of disregard and violation of the rights of others, lack of empathy, bloated self-image, manipulative and impulsive behavior. Individuals with this disorder may also exhibit: – Aggressive, violent behavior – Consistently irresponsible – Disregard for others’ needs or feelings – Disregard for the safety of self or others – Impulsive behavior – Lack of remorse for behavior – Persistent lying, stealing, using aliases, conning others – Recurring problems with the law – Repeated violation of the rights of others |
| Borderline Personality Disorder: | Characterized by a pervasive pattern of abrupt mood swings, instability in relationships, self-image, identity, behavior, and affect often leading to self-harm and impulsivity. Individuals with this disorder may also exhibit: – Frequent, intense displays of angerImpulsive and risky behavior – Intense fear of being alone or abandoned – Ongoing feelings of emptiness – Stress-related paranoia that comes and goes – Suicidal behavior or threats of self-injury – Unstable and intense relationships – Unstable or fragile self-image – Up and down moods, often as a reaction to interpersonal stress |
| Narcissistic Personality Disorder: | Characterized by a pervasive pattern of grandiosity, need for admiration, and a perceived or real lack of empathy. In a more severe expression, narcissistic personality disorder may show evidence of paranoia, aggression, psychopathy, and sadistic personality disorder, which is known as malignant narcissism. Persons with this disorder may also exhibit: – Arrogance – Belief that one is special and more important than others – Having envy of others or believing that others envy them – Exaggeration of achievements or talents – Expectation of constant praise and admiration – Failure to recognize others’ needs and feelings – Fantasies about power, success, and attractiveness – Unreasonable expectations of favors and advantages, often taking advantage of others |
Cluster C Personality Disorders
Cluster C personality disorders are characterized by anxious, fearful thinking or behavior. They include avoidant personality disorder, dependent personality disorder and obsessive-compulsive personality disorder.
| Avoidant Personality Disorder: | Characterized by pervasive feelings of social inhibition and inadequacy, extreme sensitivity to negative evaluation. Persons with this disorder may also exhibit: – Too sensitive to criticism or rejection – Feeling inadequate, inferior, or unattractive – Avoidance of work activities that require interpersonal contact – Socially inhibited, timid and isolated, avoiding new activities or meeting strangers – Extreme shyness in social situations and personal relationships – Fear of disapproval, embarrassment, or ridicule |
| Dependent Personality Disorder: | Characterized by pervasive psychological need to be cared for by other people. Persons with this disorder may also exhibit: – Difficulty disagreeing with others, fearing disapproval – Difficulty starting or doing projects independently due to lack of self-confidence – Excessive dependence on others and feeling the need to be taken care of – Fear of having to provide self-care or fend for oneself if left alone – Lack of self-confidence, requiring excessive advice and reassurance from others to make even small decisions – Submissive or clingy behavior toward others – Tolerance of poor or abusive treatment, even when other options are available – Urgent need to start a new relationship when a close one has ended |
| Obsessive-Compulsive Personality Disorder: | Characterized by rigid conformity to rules, perfectionism, and control to the point of satisfaction and exclusion of leisurely activities and friendships. Persons with this disorder may also exhibit: – Desire to be in control of people, tasks and situations, and inability to delegate tasks – Extreme perfectionism, resulting in dysfunction and distress when perfection is not achieved – Inability to discard broken or worthless objectsInflexible about morality, ethics, or values – Neglect of friends and enjoyable activities because of excessive commitment to work or a project – Preoccupation with details, orderliness, and rules – Rigid and stubborn – Tight control over budgeting and spending money – Obsessive-compulsive personality disorder is not the same as obsessive-compulsive disorder, a type of anxiety disorder. |
Personality disorders are not only grouped by category and cluster. It is also possible to classify personality disorders using additional factors such as severity of the disorder, impact on social functioning, and attribution.
Classifying personality disorders by severity uses a subthreshold (personality difficulty) as a measure of scores for personality disorder. These scores use interviews and show evidence that people with the most severe personality disorders will likely demonstrate a ripple effect of personality disturbance across the whole range of mental disorders. This is demonstrated in the table below:
Dimensional System of Classifying Personality Disorders
| Level of Severity | Description | Definition by Categorical System |
| 0 | No Personality Disorder | Does not meet actual or subthreshold criteria for any personality disorder |
| 1 | Personality Difficulty | Meets subthreshold criteria for one or several personality disorders |
| 2 | Simple Personality Disorder | Meets actual criteria for one or more personality disorders within the same cluster |
| 3 | Complex (Diffuse) Personality Disorder | Meets actual criteria for one or more personality disorders within more than one cluster |
| 4 | Severe Personality Disorder | Meets criteria for creation of severe disruption to both individual and to many in society |
There are several advantages to classifying personality disorders by severity. For instance, it takes advantage of the tendency for personality disorders to be comorbid with each other, it shows personality disorders’ influence on clinical outcomes, and it accommodates the new diagnosis of severe personality disorder, particularly severe personality disorder.
Effect on social functioning
Social functioning is affected by many other aspects of mental functions apart from personality. Whenever social functioning is impaired when it normally would not be, it is more likely to be created by a personality abnormality than by other clinical causes. The Personality Assessment Schedule prioritizes social functioning by creating a hierarchy where a personality disorder that creates social dysfunction is most important over other personality disorders.
Attribution
Often, people who have a personality disorder do not recognize that their behaviors are abnormal and will refuse treatment. This group has been termed the Type R, or people with treatment-resisting personality disorders, as opposed to the Type S or those with treatment-seeking personality disorders. These people accept that they have a personality disorder and are active in seeking treatments for improved behaviors.
Emotional stress is a condition that occurs when a person’s emotions are affected when they are stressed. There are several contributors to stress; finances, work, family life, etc. and not being able to cope with stress can produce physical and emotional symptoms. Emotional signs of stress can include:
- Depression
- Anxiety
- Irritability
- Low sex drive
- Memory and concentration problems
- Compulsive behaviors
- Mood swings
Antidepressants: Medications used to treat depression, anxiety, pain, and insomnia
- Most common are serotonin reuptake inhibitors (SSRIs), which work by increasing serotonin levels in the brain, which influences emotions, mood, and sleep.
- Common SSRIs include:
- Fluoxetine
- Citalopram
- Sertraline
- Paroxetine
- Escitalopram
- Common SSRIs include:
- Other types of antidepressants are serotonin and norepinephrine reuptake inhibitors (SNRIs), which work by reducing the absorption of serotonin and norepinephrine (neurotransmitters) in the brain cells, improving mood, and reducing anxiety and panic attacks.
- Common SNRIs include:
- Venlafaxine
- Duloxetine
- Common SNRIs include:
- Antidepressant considerations:
- Combining the newer SSRI or SNRI antidepressants with medications used to treat migraine headaches could cause a life-threatening illness called serotonin syndrome, which results in agitation, hallucinations, high fevers, and extreme changes in blood pressure.
- It is important to take antidepressant medications as prescribed to achieve therapeutic effects. Depending on the medication prescribed, it could take four weeks or more for it to reduce or alleviate symptoms.
- The medications prescribed should never be stopped abruptly as they could cause withdrawal or return of symptoms.
Anti-anxiety medications: Help reduce anxiety symptoms, such as panic attacks, extreme fear, and worry.
- Most common are benzodiazepines which can treat any generalized anxiety disorder; however, they are second line medications for the treatment of panic disorder or social anxiety disorder, which is most often treated with SSRIs or other antidepressants
- Common Benzodiazepines include:
- Clonazepam
- Alprazolam
- Lorazepam
- Common Benzodiazepines include:
- Benzodiazepine considerations:
- Benzodiazepines take effect much faster than other antidepressant medications and have the potential to cause dependency.
- Tolerance to Benzodiazepines may occur if they are taken over a long period of time, and withdrawal may occur if benzodiazepine use is stopped abruptly.
Stimulants: Increase alertness, energy, and attention, and may be used to treat narcolepsy and depression in the elderly and chronically ill who have not responded to other treatments. These medications are also used to treat Attention Deficit Hyperactive Disorder (ADHD), because they have a calming effect allowing people with ADHD to focus.
- Stimulants that treat ADHD include:
- Methylphenidate
- Amphetamine
- Dextroamphetamine
- Lisdexamfetamine Dimesylate
- Considerations:
- When taken as properly and as prescribed, there is little evidence of stimulants leading to drug abuse.
Antipsychotic medicines: Are mainly used to manage psychosis in someone who has lost touch with reality, or is experiencing auditory or visual hallucinations or delusions, which may be a symptom of a physical condition such as drug abuse or a mental disorder such as schizophrenia, bipolar disorder, or very severe depression. These medications are frequently used in combination with other medications to treat delirium, dementia, and mental health conditions such as ADHD, eating disorders, generalized anxiety disorder, obsessive-compulsive disorders (OCD), PTSD, and severe depression. There are two generations of antipsychotic medications:
- First generation (typical) and second generation (atypical) antipsychotics both work to treat symptoms of schizophrenia and the manic phase of bipolar disorder, however, several atypical antipsychotics have a broader spectrum of action than the first generation (typical) medications, and are used for treating bipolar depression or depression that has not responded to an antidepressant medication alone.
- Common first-generation (typical) antipsychotic medications include:
- Chlorpromazine
- Fluphenazine
- Haloperidol
- Perphenazine
- Second generation (atypical) antipsychotic medications include:
- Aripiprazole
- Lurasidone
- Olanzapine
- Paliperidone
- Quetiapine
- Risperidone
- Ziprasidone
- Considerations:
- First generation antipsychotic medications can also cause rigidity, persistent muscle spasms, tremors, and restlessness related to tardive dyskinesia. The symptoms will usually resolve once the medication is discontinued.
Mood stabilizers: Mainly used to treat bipolar disorder, mood swings associated with other mental disorders, and to augment the effect of other medications used to treat depression. Mood stabilizers work by decreasing abnormal activity in the brain and may also be used to treat depression, schizoaffective disorder, mental illness in children, and disorders of impulse control.
- Lithium is most often used for the treatment of mania and bipolar disorder.
- Anticonvulsant medications are also used as mood stabilizers.
- Valproic acid is often used for mixed symptoms of mania and depression or rapid cycling bipolar disorder. Other anticonvulsants used as mood stabilizers include:
- Carbamazepine
- Lamotrigine
- Oxcarbazepine
- Considerations:
- Lithium is eliminated by the kidneys, and anyone taking it should shave regular doctor visits to check the lithium levels and make sure the kidneys and the thyroid are working normally.
Special Group Considerations:
Children:
- Some medications have not been studied or approved for use with children or adolescents, however medications may be prescribed on an off-label basis. In addition to medications, other treatments such as psychotherapy, family therapy, educational courses, or behavior management should be considered, either to be tried first, with medication added later if necessary, or to be provided along with medication.
Pregnant Women:
There is limited research on the use of psychiatric medications during pregnancy. Decisions on treatments during pregnancy should be based on a woman’s needs and weighing the benefits and risks of all available options, including psychotherapy. Risks from the use of antidepressants also needs to be balanced with the risks of stopping medication; if a mother is too depressed to care for herself and her child, both may be at risk for harm.
Although research is limited, some drugs are known to cause birth effects during pregnancy. For example:
- Mood stabilizers are known to cause birth defects.
- Benzodiazepines and lithium have been shown to cause floppy baby syndrome where the baby is drowsy and limp and cannot breathe or feed well.
- Benzodiazepines may cause birth defects if they are taken during the first trimester.
- Antipsychotic medications taken during pregnancy can cause birth defects.
Elderly:
People over the age of 65 are at increased risk of medication interactions (they are more likely to take multiple medications), missing doses of medications, or taking too many medications at once. Older adults also tend to be more sensitive to medications. Because of their sensitivity, lower or less frequent doses may be needed for the elderly. Before starting a medication, older people and their family members should discuss whether a medication could affect alertness, memory, or coordination, and how to help ensure that prescribed medications do not increase the risk of falls.
Several medications have been linked to suicidal behavior, and this has prompted the United States Food and Drug Administration (FDA) to require a black box warning on several prescription medications which include analgesics, anticonvulsants, and antidepressants. ⁵
| Antidepressants | Several studies have shown a link between antidepressant use in childhood and teenagers to self-destructive behavior. Such an association has also been reported in adults. |
| Anticonvulsants | Reports of suicidal behavior after initiating anticonvulsant therapy have persisted for over 2 decades. Drugs like lamotrigine, gabapentin, tiagabine, and oxcarbazepine have been linked to an increased risk for self-harm or even violent death. |
| Analgesics | The analgesic, tramadol, has also been associated with a risk of self-harm. In 2010, the FDA added a warning to the label that the drug has the potential of causing self-harm. |
| Smoking Cessation Medications | One of the newer anti-smoking drugs, varenicline is also known to be associated with self-injurious behaviors and is not recommended as first-line therapy for people who want to quit smoking or have a history of mental illness. |
| Glucocorticoids and Anabolic Steroids | It has been known for many years that both glucocorticoids and several anabolic steroids can induce rage and self-destructive behavior. Many professional wrestlers have committed suicide over the past 3 decades, and it is believed that this is because of anabolic steroid use. |
Bipolar Disorder:
People who have bipolar disorder are at remarkably high risk for suicidal behavior, especially females whose onset of symptoms appeared early in life. In addition to the manic phase and impulsive behavior, people with bipolar disorder can also develop severe depression that poses a risk for suicide. Other comorbid factors that increase the risk of suicidal behavior in people with bipolar disorder include the presence of an anxiety disorder, and a family history of suicide. An effective treatment that is commonly used in bipolar disorder and has anti-suicidal effects is Lithium; a mood stabilizer that is a used to treat or control the manic episodes and depression associated with bipolar disorder. One caveat is that lithium has an exceptionally low therapeutic index, and its use must be closely monitored because lithium toxicity can occur at levels that are close to being therapeutic. Compliance with lithium therapy is also a major issue among bipolar patients because Lithium can take several weeks for it to start to take effect, even when it is taken consistently to treat bipolar disorder.
Schizophrenia:
People with schizophrenia are also at remarkably high risk for suicide. Often, people with schizophrenia experience delusions and auditory hallucinations that may tell them to harm themselves. Schizophrenia may also lead to severe paranoia and fear which could cause one to self-harm. Self-medication with drugs and alcohol is also common and may contribute to the high risk of suicides. Several studies show that the use of the atypical antipsychotics in schizophrenia is associated with a decrease in suicide attempts in schizophrenia. The evidence favoring clozapine is strongest which is, in fact, the only medication approved by the FDA for preventing suicides in these patients. Clozapine works by changing the actions of chemicals in the brain and is also used to treat psychosis in those who are treatment resistant.
Obsessive Compulsive Disorder and other Anxiety Disorders:
Generalized anxiety and obsessive-compulsive disorders (OCD) can cause symptoms that may increase suicide risk. People with phobias can develop severe symptoms, such as feeling scared, frightened, or terrorized. Other people may experience panic attacks, anxiety, or a sense of doom. Many people with phobias often are not able to control their behavior and may become incapacitated. Studies in college students have also shown an association between OCD and suicide. The risk of suicide in OCD is also increased when someone has a substance use disorder or a comorbid personality disorder. Most often, someone with OCD or other anxiety disorders will be prescribed antidepressant medications or cognitive behavioral therapy (CBT). Obsessive compulsive disorder has a cycle, which includes obsessions, anxiety, compulsions, and relief. Cognitive behavioral therapy, a type of psychotherapy, gives someone suffering from OCD the right resources to think, act, and react to unhealthy thoughts and habits. The goal is to replace negative thoughts with productive thoughts. It is important to note, that if antidepressants are used, the effectiveness of each antidepressant is dependent on one’s body chemistry, the dosage, and the frequency of use of the medication. Antidepressant medications, when taken as prescribed, may take up to 12 weeks to have a therapeutic response.
Post-traumatic stress disorders (PTSD):
Post-traumatic stress disorders can also increase the risk of suicide. Many people with PTSD are survivors of trauma, emotional, physical, or sexual abuse, and suffer from nightmares and flashbacks. Veterans of the wars in Afghanistan and Iraq have been known to have exceedingly high rates of PTSD with many struggling to maintain normalcy in daily life functions. These individuals have recorded extremely high rates of suicides. Today, most veterans are screened for PTSD, and early adjustment to normal life is necessary to prevent the risk of self-harm. When treatment is needed for PTSD, the main treatments provided are medications, and psychotherapy (talk therapy). Most often, a person with PTSD may be prescribed antidepressant medication, which may help control PTSD symptoms such as sadness, worry, anger, and feelings of emptiness. Other medications may be helpful for treating specific PTSD symptoms, such as sleep problems and nightmares.
Substance Abuse:
Substance abuse is known to lead to self-destructive behavior. Even people in a drug recovery program are at risk for self-harm, especially those with chronic pain, access to a firearm, and access to other street drugs. A person who abuses illicit drugs or prescription medications can develop depression and suicidal behavior. In many circumstances, depression that occurs during the withdrawal period has led to suicidal behaviors. Similarly, people who abuse drugs or alcohol may suffer consequences that include job loss, separation or divorce, and loss of a home. These losses can result in depression and suicide.
Dementia and Delirium:
Dementia and delirium often lead to memory loss, delusions, hallucinations, disorientation, and poor judgment. These symptoms frequently lead to self-harm. Many dementia patients feel that they have lost control of their minds and end up committing suicide.
Traumatic Brain Injury:
Traumatic brain injury has been associated with an increased risk of suicide. Studies on military personnel and sports athletes with repeated head injuries and concussions have noted the presence of depression, PTSD, and increased risk of suicidal behavior.
Bulimia is known to be linked to a higher risk of suicidal behavior. Predisposing factors include the use of stimulants, childhood abuse, family history of mental disorders, loneliness and isolation, and difficulty interacting with people in general. Along with suicidal behavior, some experts believe that both a family history of suicide and genetic factors may also be high-risk factors for suicide in bulimics. ⁷
Chronic Illness and Physical Illness:
Chronic illnesses and physical illnesses that are severe, debilitating, or incapacitating are common reasons for suicide. For example, a significant number of patients with end-stage renal disease commit suicide. Other chronic disorders that increase the risk of suicide include chronic obstructive pulmonary disease, dementia, cancer, quadriplegia, heart failure, multiple sclerosis, and severe burns to the body. A more recent study indicates that patients with fibromyalgia and migraines also have a higher risk of suicide and the risk is further increased in the presence of depression.
Loss of a Loved One:
In some cases, acute life events may trigger suicidal behavior. This may be due to the loss of a spouse, divorce, end of an interpersonal relationship, loss of a pet or even loss of employment. The acute loss can be agonizing and traumatic, leading some people to commit suicide.
Financial Instability:
In the United States, financial loss or economic instability is a common cause of suicide. Over the past decade, many reports have surfaced of people who have killed not only themselves but their entire families because of financial strain. For instance, some people have lived beyond their financial means, resulting in financial catastrophe, while others have committed suicide in response to fraud and to prevent sentencing and long jail sentences. Suicides due to financial loss are more common in adult men than in women. However, simply being poor or born into poverty does not increase the risk of suicide. ¹⁷
Age
The risk of suicide varies by gender, age, ethnicity, and race. Suicide is known to occur in people of all ages, including high school students, but the highest rate of suicide is known to occur in seniors older than age 75. ¹⁷
- Among ethnic groups, the highest risk of suicide is in Alaskan natives, American Indians, and non-Hispanic whites. While the highest risk of suicide among Alaskan natives is in adolescents, in non-white Hispanics, the risk of suicide continues to increase with advancing age.
- In men, suicide risk is highest for those between ages 50 to 85 (30 deaths per 100,000).
- In the United States, the highest suicide rates are among Whites followed by American Indians and Alaskan natives. Suicide rates are much lower in African Americans, Asians, and Pacific Islanders.
- In women, the suicide risk is highest between ages 60 to 65 (5 to 7 deaths per 100,000).
- Women tend to have a much higher rate of suicide attempts, but men have a much higher rate of suicide completion.
- Overall, the highest risk for suicide is in men over the age of 65.
- Seventy-five percent of all suicides are seen in white males.
- Suicide is the third leading cause of death in adolescents and teens between ages 15 to 24.
Occupation
Professions associated with a high rate of suicide include law enforcement and public safety officers (firemen, emergency medical personnel, physicians, etc.). These professionals often have long, irregular work hours, witness various types of injuries, and have access to guns or potent drugs and narcotics which places them at high risk for suicide. Some of these professionals are also at risk for alcohol abuse, which is often used as a coping strategy to a stressful event. Physicians have a particularly high rate of divorce because of job-related stress and the reluctance to seek help. ²⁰
Having the birthday blues, where an individual attempts suicide on or around their birthday, is a phenomenon that is resultant of psychological stress, depression, loss, increased drug and alcohol use, or lack of sense of accomplishment. Males between ages 25 to 54 are most likely to commit suicide on their birthday than any other age group. Often, they do not have any diagnosed mental health history, and will not seek help when they are feeling suicidal.
Suicides also tend to have seasonal variability with most suicides occurring during spring. Despite the belief that year-end holidays are a frequent period of suicide, data does not support that idea. The month of May usually has a high rate of suicide, and it is believed those who suffer from depression may have a dampened mood during the winter months, however, with the arrival of spring, some people with depression may remain depressed or have an increase in depression, resulting in attempted suicide.
There has been a lot of debate on the use of universal screening for depression in primary care. The overall feeling is that such screening should only be undertaken if there is a strong commitment to provide treatment and follow up. There are many screening tools for suicide, but there is not one screening tool that is applicable to all people who are at risk for suicide. In addition, a healthcare professional should not rely solely on a screening tool to evaluate a risk for suicide, but also consider history with a detailed assessment of past mental health history. ¹⁴˒²²
The idea for universal screening for depression poses that everyone who presents to a primary care provider should be screened for depression. Often, people are screened for depression in the primary care setting, however, there is lack of follow-up and treatment. It is imperative that a healthcare professional screen for depression and provide treatment and follow-up care because continued care improves health outcomes. Screening alone without any follow up is not recommended because it does not prevent or reduce the risk of suicide.
Instead of universal screening, some healthcare professionals have suggested targeted screening. In targeted screening, the healthcare provider screens for depression and suicide risk based on established criteria. The following criteria have been identified in populations at risk for depression and suicide and warrant evaluation:
- Anyone with a familial history of depression
- Anyone with chronic pain
- Anyone with two or more chronic diseases
- Constant fatigue
- Current or history of substance abuse
- Elderly and living alone
- Loss of sexual interest
- Postpartum depression
- Sleep disturbances
- Socially isolated or lonely
- Sudden changes in life such as divorce or death
- Under severe financial strain
When the screening tools are used appropriately, they can be useful in helping healthcare professionals recognize depression, and when the screening tools are accompanied by a commitment to follow up and treatment, better outcomes are achieved. However, screening tools should be used by healthcare professionals who are committed to using the information from the screening test to provide enhanced care. ¹⁴˒²²
Now there is little evidence to support screening the population at large. In fact, in people without any psychiatric history, the role of screening remains debatable. Each hospital or organization has its own protocols when it comes to the use of suicide prevention tools. No study has ever shown that one tool is better than the other.
If a screening assessment for suicide prevention and depression is initiated, then it must also have effective follow-up and treatment. Once someone has been diagnosed with depression and is at high risk for suicide, there must be a system in place for treatments such as psychotherapy and/or antidepressant medications. If close follow up and treatment is not available, then the healthcare professional must make a recommendation for referral and follow-up.
The costs of screening for suicide are minimal. Except for some time and the use of questionnaires, there are no other exorbitant costs. Data has shown that on average, less than 20% of primary care physicians screen adolescents or seniors for suicidal risk factors.
Some healthcare professionals suggest using an alternative approach to preventing suicide other than identifying people at risk. The reason is that many models of screening have not shown to be effective in suicide prevention, because there may be a lapse in follow-up care. Suicide has been strongly linked to social problems, and the rates are generally much higher in local communities which lack a cohesive social fabric or when people are left out of mainstream society. Thus, it is suggested that other factors be improved to reduce suicide risks, such as housing, job opportunities, and ease of access to mental health care professionals and prescription medications. Unfortunately, many of the social factors far outreach the ability of most primary health care providers to manage. In addition, there is also a significant cost that accumulates with making changes in the social structure.
The Joint Commission compiled a list of useful resources to meet the needs of assessing for depression and suicidal ideation. The list complied was created by Joint Commission staff and suicide prevention experts who verified that the instruments met the requirements of the standards for risk assessment. The resources to create the instruments were compiled from key stakeholders including national organizations, federal and state agencies, professional associations, relevant academic institutions, peer reviewed publications and private entities. The following is a brief overview of some of the tools approved by Joint Commission:
| Ask Suicide-Screening Questions (ASQ) National Institute of Mental Health: | The ASQ toolkit was developed and validated by a team from the National Institute for Mental Health (NIMH) following a 2008, multisite study. Ask Suicide-Screening Questions is a four-item suicide-screening tool designed to be used for people ages 10–24 in emergency departments, inpatient units, and primary care facilities. A Brief Suicide Safety Assessment is available to be used when patients screen positive for suicide risk on the ASQ. |
| The Beck Scale for Suicide Ideation (BSI): | The BSI is a 21-item self-report instrument for detecting and measuring the current intensity of a person’s specific attitudes, behaviors, and plans to commit suicide during the past week. The first 19 items comprise of three options graded according to the intensity of the suicidal ideation and rated on a 3-point Likert scale ranging from 0 to 2. These ratings are then added to identify a total score, which ranges from 0 to 38. The individual items assess characteristics such as wish to die, desire to make an active or passive suicide attempt, duration and frequency of ideation, sense of control over trying, number of deterrents, and amount of actual preparation for a contemplated attempt. The last two items assess the number of previous suicide attempts and the seriousness of the intent to die associated with the last attempt. |
| The Patient Health Questionnaire-9 (PHQ-9) Depression Scale: | The Patient Health Questionnaire-9 is a validated widely used nine-item tool that is used to diagnose and monitor the severity of depression. Most specifically, question 9 screens for the presence and duration of suicide ideation. It is available in Spanish and other languages and has also been modified for the adolescent population. |
| The 19-item Scale for Suicide Ideation – Worst (SSI-W): | The SSI-W is a rating scale that is administered by an interviewer. It measures the intensity of a person’s specific attitudes, behaviors, and plans to commit suicide during the time that they were the most suicidal. The instrument was developed to obtain a more accurate estimate of suicide risk. Each SSI-W item apprises of three options graded according to the suicidal intensity on a 3-point Likert scale ranging from 0 to 2. The ratings are then added to equal a total score, which ranges from 0 to 38. Individual items assess characteristics such as wish to die, desire to make an active or passive suicide attempt, duration and frequency of ideation, sense of control over trying, number of deterrents, and amount of actual preparation for a contemplated attempt. The SSI-W takes approximately 10 minutes to administer. |
| Suicide Behavior Questionnaire-Revised (SBQ-R): | The SBQR is a four-item self-report questionnaire that asks about future anticipation of suicidal thoughts or behaviors as well as past and present ones, and includes a question about lifetime suicidal ideation, plans to commit suicide, and actual attempts. The first item evaluates lifetime ideation and attempt, the second item assesses frequency of suicidal ideation in the past 12 months, the third item explores suicidal threats, and the fourth item evaluates the likelihood of future suicidal behavior. |
| The SAFE-T: | The SAFE-T tool can be used in an outpatient setting and does offer a good insight into the extent and nature of suicidal thoughts and harmful behavior. The SAFE-T explores the following: What is the suicidal ideation, its intensity, frequency, and duration within the past 48 hours and over the past 4 weeks? It also determines the most serious or worst harmful thought. Planning of the suicide, location, time, availability, and if any preparations have been made. It provides information on past behaviors such as past suicide attempts and any aborted attempts. It also asks if the individual has rehearsed any events like loading or pointing a gun or tying a noose. Has the individual visited the location like a bridge or waterfall? The intent and extent when the individual is likely to carry off the plan is also assessed. The SAFE-T also gives insight into where the individual is serious or ambivalent about self-harm. |
| The Columbia-Suicide Severity Rating Scale (C-SSRS): | The C-SSRS is another tool that can be utilized in outpatient settings to assess for the presence of harmful behavior. The C-SSRS also assess any known suicide attempts and assesses suicide ideations and behaviors. Like the SAFE-T it can be used as an initial screen. The C-SSRS Triage version features questions that help determine whether a person is at risk for suicide. There are brief versions of the C-SSRS often used as a screening tool (first two questions) that, based on a person’s response, can lead to the administration of the additional questions. |
No one instrument is 100% sensitive, and choosing one depends on personal preference and experience. When initiating a screening program for suicide, it is important to have access to effective treatment and follow up. Other considerations include:
- Understand the nature of depression
- Making a commitment to routinely assess for depression and suicidal ideation
- Refer patients timely to the appropriate specialists
- Utilize resources to prevent suicide such as hotlines
- Conduct repeat screening to identify any ongoing depression
Because depression has no cure and relapse is common, rescreening should be continued at regular intervals. ²⁶
All healthcare workers who screen for suicide should be aware that the screening tools are not 100% guaranteed to identify suicidal behavior and can lead to false identifications. This can result in costly health care. It should also be noted, that often, people who are suicidal may not exhibit any symptoms of suicidal thoughts or depression and may not seek medical or psychiatric care. ²⁶
An inquiry on suicide should be included in every mental health assessment, and the healthcare professional should keep in mind the person’s age and developmental level when conducting the exam. It is important to obtain a thorough history, especially regarding thoughts and self-destructive behavior. ¹⁴Even though people may talk about suicide, few commit suicide, however, it also poses true that people who have suicidal ideation are more likely to exhibit suicidal behavior. In some cases, the assessment of one’s mental status may provide a clue to the individual’s potential for self-harm. The mental health assessment should include observations of the following:
| Appearance: | Depressed people may appear unclean and unkempt. The clothing may not be ironed, or it may be dirty. The physical exam may reveal scars or rope burns on the hands, wrists, or neck. Often these people may have multiple injuries to their body. The healthcare professional should consider assessing the full body if the initial assessment reveals marks or scars that suggest self-harm. |
| Affect: | The risk of suicide is often higher in people who appear very anxious or depressed. One may also exhibit a flat affect or no emotions at all. |
| Thoughts: | People with an intent to self-harm may have several types of abnormal thoughts which include the following: · Hallucinations: Some depressed people may develop hallucinations that may be telling them to kill themselves. Most of these hallucinations are auditory. · Delusions: Sometimes a person may develop a false belief (delusion) that everyone hates them or wants them dead. And if they die, the family will be better off. · Obsessions can sometimes be quite intense and can lead the individual to take his or her own life. |
| Judgment, Insight, and Intellect: | Assessing a person’s judgment is critical. The healthcare professional should try and determine how the person handles stress, and whether they have an impairment in decision making. Assess for memory and orientation which are often abnormal in patients with self-destructive behaviors. |
A list of signs that may be indicative of impending suicide include the following:
- Constantly dwelling on the past, losses, or defeats, and making statements like the world is better off without them.
- Constantly talking about suicide or death: Many people planning suicide often have a plan in mind and may have planned to buy a weapon.
- Experiencing paranoia, delusions or hallucinations telling them to die.
- Having a constant preoccupation with death or a sense of doom.
- Having a general clinical impression of someone who is suicidal or depressed.
- Having a history of depression.
- Having a strong family history of suicide.
- Having a sudden negative event in life, such as losing a job, divorce, or death of a family member or spouse.
- Having recently been discharged from a mental health facility.
- If the person is under the influence of alcohol, prescription medications or other illicit mind-altering drugs.
- If the person is known to possess a weapon, especially a gun.
- Lack of coping mechanisms.
- Living alone or isolated.
- People who state that they may not be around much longer, and say goodbye to family or friends, arranging a funeral plan, making a will, or writing a suicide note.
Similarly, there are several activities that have been associated with an intent to commit suicide including:
- Buying a weapon like a gun, rope, or chemicals
- Getting all the house and family affairs together
- Going to the emergency room or visiting a healthcare provider
- Making a will
- Seeing friends and family unexpectedly
- Visiting a primary care physician. A significant number of people see their primary care physician within 3 weeks of committing suicide.
- Writing a suicide note
Several people go to the emergency department or visit their primary health care provider with complaints of ailments within a few weeks prior to committing suicide. Often, they rarely mention suicidal ideations but may have vague physical complaints. Thus, the healthcare professional must obtain a good mental health history beyond just the chief complaint. The healthcare provider should also try to ascertain protective factors against suicide by assessing if:
- The person has any long-term plans or events such as a wedding, birth of a child, etc.
- The person has called any crisis hotlines in the past.
- The person has children, and their interactions with them.
- The person is involved in a relationship or social network of family, friends or colleagues, and frequency of communicating with them.
- The person is already receiving treatment for depression.
- The person is religious.
- The person is seeing a therapist.
- The person owns a weapon.
A clear and complete evaluation and clinical interview provide the information upon which to base a suicide intervention. Although risk factors offer major indications of the suicide danger, nothing can substitute for a focused patient inquiry. However, although all the answers a person gives may be inclusive, a healthcare provider often develops a visceral sense that someone is contemplating committing suicide. ⁵˒²⁶
The healthcare professional should first determine whether the person has any thoughts of hurting themself. Suicidal ideation is highly linked to completed suicide. Some inexperienced healthcare providers have difficulty asking this question. They fear the inquiry may be too intrusive or that they may provide the person with an idea of suicide. Most people appreciate the question as evidence of the healthcare professional’s concern. A positive response requires further inquiry.
If suicidal ideation is present, the next question must be about any plans for suicidal acts. In general, more specific plans indicate greater danger for suicide. Although vague threats such as a threat to commit suicide sometime in the future are the reason for concern, responses indicating that the person has purchased a gun, has ammunition, has made out a will, and plans to use the gun are more dangerous. The plan demands further questions. If the person envisions a gun-related death, determine whether they have the weapon or access to it.
In further inquiry, the healthcare professional should determine what the individual believes their suicide would achieve. This suggests how seriously the person has been considering suicide and the reason for death. For example, some believe that their suicide would provide a way for family or friends to realize their emotional distress. Others see their death as a relief from their own physical pain. Still others believe that their death would provide a heavenly reunion with a departed loved one. In any scenario, the healthcare professional has another gauge of the seriousness of the planning.
Any question of suicide also must be coupled with an inquiry into the person’s potential for homicide. Suicide is often thought to represent aggression turned inward, whereas homicide represents aggression turned outward. Because suicide constitutes an aggressive act, the question regarding homicidal tendencies must be asked.
Collateral questions should be asked based on the reviewed risk factors. These questions deal with any family members or friends who have killed themselves and include questions about symptoms of depression, psychosis, delirium and dementia, losses (especially recent ones), and substance abuse.
The treatment of a person who is suicidal involves a 2-phase process. The first phase includes intervention to assure the person’s safety. The type of intervention conducted is based on the assessment of risk factors during the clinical inquiry. The second phase includes treatment that is aimed at diagnosing and treating the underlying mental disorder. ⁵
First Phase of Intervention
In many cases, a swift intervention can prevent a person from committing suicide. It is critical to act when the risk for suicide is recognized. Based on the clinical assessment and all the information available, if the person is indeed suicidal, the intervention should consist of multiple steps.
- , 911 should be called. If appropriate, the healthcare professional should involve family or friends, as they can remain with the patient while treatment arrangements are made.
- The healthcare professional should also remove anything that the individual may use to hurt themself with, such as sharp objects or anything else deemed to be dangerous, like medications. People who attempt to commit suicide with prescribed medications represent one of the greatest clinical challenges. The dilemma involves the fact that psychotropic medications alleviate mental illness symptoms, yet some people will use the very same medications to commit suicide. To reduce the risk of a suicide attempt, the healthcare provider should ask the individual if they have access to any weapons, such as knives, pills, or firearms, and they should be secured away from the person.
- The person who is suicidal should be treated in a secure, safe, and highly supervised location. Inpatient care at a hospital offers one of the best settings. Most managed care companies recognize the medical necessity of hospitalization in situations in which the suicide danger is acute.
Second Phase of Intervention
After the initial intervention, which usually includes hospitalization, it is critical that there be in place an ongoing management treatment plan.
- The heart of the second phase of the intervention is addressing the underlying cause of the self-destructive behavior. For instance, if the individual has selected suicide to escape physical pain, then a comprehensive pain management program must be initiated. If the individual is depressed, then the depression must be treated with medication and psychotherapy. If the suicide attempt was in response to struggling with destructive hallucinations or delusions of schizophrenia, then these must be aggressively treated. The key remains an accurate assessment and diagnosis followed by a comprehensive treatment plan.
- Once the person is safe as an inpatient or outpatient, a formal treatment plan should be established. If person during the assessment a person is deemed to be at high risk for suicide, they should immediately be evaluated by a mental health professional. Every state has laws and procedures regarding this process which must be incorporated into the clinical practice when addressing people at high suicide risk.
- Once the treatment is initiated and before the person is discharged, the following additional safety measures must be established:
- Help develop internal coping strategies such as exercise or developing a hobby.
- Promote social support by having a family member, social worker, or friend call to check on the person.
- Utilize the help of healthcare professionals to follow up on therapy.
- Provide the individual with the National Suicide Prevention Lifeline.
- Tell the person to call 911 if they develop any suicidal thoughts or behaviors.
- Tell family members/caregivers to take the person to the emergency room if mental health decompensation occurs.
If a person has acute psychiatric symptoms like paranoia, hallucinations, extreme anxiety or depression, pharmacological therapy may be needed. After the patient’s acute symptoms have been managed, the choice of further treatment depends on the specific mental illness. In most cases, psychotherapy is recommended to treat the thoughts of self-harm. However, it is important to note that despite these interventions, many people do commit suicide. It is important to involve the patient’s family, friends, and social worker in the long-term management and care. ⁶˒²⁶
While drug treatment is useful for the management of acute symptoms like hallucinations, psychosis, or depression, psychotherapy is essential for long-term management. Psychotherapy is a general term for treating mental health problems by talking with a psychiatrist, psychologist, or other mental health provider. Psychotherapy can be helpful in treating most mental health problems, including addictions, anxiety disorders, eating disorders, mood disorders, personality disorders, and schizophrenia. There are several effective types of psychotherapy. Some work better than others in treating certain disorders and conditions. Although many types of therapies exist, some psychotherapy techniques proven to be effective include:
| Acceptance and Commitment Therapy | Helps an individual become aware of and accept thoughts and feelings. and commit to making changes, increase their ability to cope and adjust to situations |
| Cognitive Behavioral Therapy (CBT) | Helps an individual identify unhealthy, negative beliefs and behaviors and replace them with healthy, positive ones |
| Dialectical Behavior Therapy | Teaches behavioral skills to help an individual handle stress, manage emotions, and improve relationships with others |
| Interpersonal Psychotherapy | Focuses on addressing problems with relationships with other people to improve and interpersonal skills, namely how and individual relates to others, such as family, friends, and colleagues |
| Psychodynamic and Psychoanalysis Therapies | Focus on increasing awareness of unconscious thoughts and behaviors, developing new insights into motivations, and resolving conflicts |
| Supportive Psychotherapy | Reinforces the ability to cope with stress and difficult situations |
Often, it takes several regular sessions spread over many months or even years to effectively treat a condition, which can be costly. Unfortunately, psychotherapy may not be covered under insurance for treatment. ²⁶
Healthcare professionals must work with the individual’s family and friends, as well as with the other patients who knew the deceased.
Upon learning of the death of a person being treated or was treated for suicidal ideation or behaviors, the healthcare professional should take time to meet with the family. Often, family members appreciate the healthcare professional’s interest and the opportunity to voice their feelings and reactions. In some situations, the family may have expected the outcome. In others, they may be hurt and angry. The healthcare professional’s job is to be responsible and responsive to them. This intervention may require more than one session. It is important for the healthcare professional to be available to family members, to listen to them, and to share their loss.
If the patient who committed suicide was an inpatient, convening a group meeting and discussing the other patients’ reactions is important. Often, other patients knew the deceased person. Without violating confidentiality, the healthcare professional should provide extra attention to these patients. This could include sessions to allow them to express their reactions to death and loss. The staff should also have an opportunity to discuss their feelings. Finally, the healthcare provider must take the time to review and discuss the event, and have an opportunity to recover and heal, as they also require sympathy and support.
Prior to discharging patients with depression, anxiety, or suicidal ideations, it is important to provide them with resources and referrals. ⁵
- The National Suicide Prevention Lifeline operates 24/7 and has always trained counselors available. They can be contacted at the following numbers:
- 1-800-273-TALK (1-800-273-8255), 1-800 Suicide (1-800-784-2433)
- Text Telephone: 1-800-799-4TTY (1-800-799-4889)
- Military Veterans Suicide Hotline: 1-800-273-TALK (Press 1)
- Suicide Hotline in Spanish: 1-800-273-Talk (Press 2)
- LGBT Youth Suicide Hotline: 1-866-4-U-TREVOR
- The patient should be asked to contact the US Substance Abuse and Mental health Services administration online and ask for FREE wallet cards which provide information about the National Suicide Prevention Lifeline.
- The Friendship Line is free and available to people over the age of 60. It operates 24/7 and can be reached at 1-800-971-0016. The Friendship Line helps seniors who feel lonely, depressed, or are contemplating suicide.
Finally, the patient should be provided with the names of local mental health care professionals who can be reached in case of an emergency.
Suicide is one of the most important actions that healthcare professionals must address. The healthcare professional’s assessment and intervention remain a critical step to saving a person’s life. The first step is to prevent harm to the person who is suicidal. The second step is to treat the cause of the behavior that is causing suicidal ideations. Once a person is deemed to be at risk for self-harm, a referral must be made to a mental health professional. The main treatment to reduce the risk of suicide is psychotherapy, and medications when necessary.
Having a collaborative, interdisciplinary team that includes mental health and healthcare professionals will greatly improve the treatment regimen and path to recovery for the mentally ill person. For instance, the Nurse Practitioner or psychiatry-trained Registered Nurse can screen patients for suicide risk using validated screening tools. Communicating these findings with the mental health professional can help patients receive appropriate support to decrease their risk of suicide. Similarly, the community nurse, specialty-trained social worker, and case manager can help monitor and follow up on those identified at the highest risk of suicide to ensure they follow up with the treatment plan advised and that their needs outside of medical therapy are met. All healthcare professionals should include family members in the treatment plan when appropriate, and they should be educated on the signs of depression, and suicidal ideation. With appropriate screening, treatment regimens for the person who is suicidal, and therapy to develop coping skills, the at risk or depressed person could have an improved outcome and reduced suicidal risk.
- Agrrawal, P., Waggle, D., & Sandweiss, D. H. (2017). Suicides as a response to adverse market sentiment (1980-2016). PLOS ONE, 12(11), e0186913. https://doi.org/10.1371/journal.pone.0186913
- Ahn, J., Lee, J., & Jung, Y. (2018). Predictors of suicide attempts in individuals with eating disorders. Suicide and Life-Threatening Behavior, 49(3), 789-797. https://doi.org/10.1111/sltb.12477
- Anderson, J., Mitchell, P. B., & Brodaty, H. (2017). Suicidality: Prevention, detection, and intervention. Australian Prescriber, 40(5), 162-166. https://doi.org/10.18773/austprescr.2017.058
- Anestis, M. D., Selby, E. A., & Butterworth, S. E. (2017). Rising longitudinal trajectories in suicide rates: The role of firearm suicide rates and firearm legislation. Preventive Medicine, 100, 159-166. https://doi.org/10.1016/j.ypmed.2017.04.032
- Ballard, E. D., & Zarate, C. A. (2018). Preventing suicide: A multicausal model requires multimodal research and intervention. Bipolar Disorders, 20(6), 558-559. https://doi.org/10.1111/bdi.12656
- Betz, M. E., Brooks-Russell, A., Brandspigel, S., Novins, D. K., Tung, G. J., & Runyan, C. (2018). Counseling suicidal patients about access to lethal means: Attitudes of emergency nurse leaders. Journal of Emergency Nursing, 44(5), 499-504. https://doi.org/10.1016/j.jen.2018.03.012
- Depression (major depressive disorder) – Symptoms and causes. (2018, February 3). Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/depression/symptoms-causes/syc-20356007
- Dickerson, F., Origoni, A., Schweinfurth, L. A., Stallings, C., Savage, C. L., Sweeney, K., Katsafanas, E., Wilcox, H. C., Khushalani, S., & Yolken, R. (2018). Clinical and serological predictors of suicide in schizophrenia and major mood disorders. The Journal of Nervous and Mental Disease, 206(3), 173-178. https://doi.org/10.1097/nmd.0000000000000772
- Dueweke, A. R., & Bridges, A. J. (2018). Suicide interventions in primary care: A selective review of the evidence. Families, Systems, & Health, 36(3), 289-302. https://doi.org/10.1037/fsh0000349
- El-Den, S., O’Reilly, C. L., & Chen, T. F. (2015). A systematic review on the acceptability of perinatal depression screening. Journal of Affective Disorders, 188, 284-303. https://doi.org/10.1016/j.jad.2015.06.015
- Goodfellow, B., Kõlves, K., & Leo, D. (2018). Contemporary definitions of suicidal behavior: A systematic literature review. Suicide and Life-Threatening Behavior, 49(2), 488-504. https://doi.org/10.1111/sltb.12457
- Kann, L., McManus, T., Harris, W. A., Shanklin, S. L., Flint, K. H., Queen, B., Lowry, R., Chyen, D., Whittle, L., Thornton, J., Lim, C., Bradford, D., Yamakawa, Y., Leon, M., Brener, N., & Ethier, K. A. (2018). Youth risk behavior surveillance — United States, 2017. MMWR. Surveillance Summaries, 67(8), 1-114. https://doi.org/10.15585/mmwr.ss6708a1
- Lesage, A., Tra, C., Rahme, E., Renaud, J., Thibodeau, L., & Séguin, M. (2017). Innovative prospects for suicide prevention and action opportunities for the public health agency of Canada and the Government of Canada. Canadian Journal of Community Mental Health, 36(2), 205-237. https://doi.org/10.7870/cjcmh-2017-023
- Lopez-Morinigo, J., Fernandes, A. C., Shetty, H., Ayesa-Arriola, R., Bari, A., Stewart, R., & Dutta, R. (2018). Can risk assessment predict suicide in secondary mental healthcare? Findings from the south London and Maudsley NHS Foundation Trust biomedical research centre (Slam BRC) case register. Social Psychiatry and Psychiatric Epidemiology, 53(11), 1161-1171. https://doi.org/10.1007/s00127-018-1536-8
- Nelson, H. D., Denneson, L. M., Low, A. R., Bauer, B. W., O’Neil, M., Kansagara, D., & Teo, A. R. (2017). Suicide risk assessment and prevention: A systematic review focusing on veterans. Psychiatric Services, 68(10), 1003-1015. https://doi.org/10.1176/appi.ps.201600384
- NIMH » suicide prevention. (n.d.). NIMH » Home. https://www.nimh.nih.gov/health/topics/suicide-prevention/index.shtml
- Okolie, C., Dennis, M., Simon Thomas, E., & John, A. (2017). A systematic review of interventions to prevent suicidal behaviors and reduce suicidal ideation in older people. International Psychogeriatrics, 29(11), 1801-1824. https://doi.org/10.1017/s1041610217001430
- Padmanathan, P., Carroll, R., Biddle, L., Derges, J., Potokar, J., & Gunnell, D. (2016). Suicide and self-harm related internet use in patients presenting to hospital with self-harm: A cross-sectional study. The Lancet, 388, S2. https://doi.org/10.1016/s0140-6736(16)32238-3
- Personality disorders – Symptoms and causes. (2016, September 23). Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/personality-disorders/symptoms-causes/syc-20354463
- Pidd, K., Roche, A., Cameron, J., Lee, N., Jenner, L., & Duraisingam, V. (2018). Workplace alcohol harm reduction intervention in Australia: Cluster non-randomized controlled trial. Drug and Alcohol Review, 37(4), 502-513. https://doi.org/10.1111/dar.12660
- Schizophrenia – Symptoms and causes. (2020, January 7). Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/schizophrenia/symptoms-causes/syc-20354443
- Screening for suicide risk: Recommendation and rationale. (2004). Annals of Internal Medicine, 140(10), 820. https://doi.org/10.7326/0003-4819-140-10-200405180-00014
- Shin, H., Kim, H. J., Kim, S., Choi, S., Oh, H., & Lee, B. (2018). Should let them go? Study on the emergency department discharge of patients who attempted suicide. Psychiatry Investigation, 15(6), 638-648. https://doi.org/10.30773/pi.2018.04.15
- Stone, D. M., Simon, T. R., Fowler, K. A., Kegler, S. R., Yuan, K., Holland, K. M., Ivey-Stephenson, A. Z., & Crosby, A. E. (2018). Vital Signs: Trends in state suicide rates — United States, 1999–2016 and circumstances contributing to suicide — 27 states, 2015. MMWR. Morbidity and Mortality Weekly Report, 67(22), 617-624. https://doi.org/10.15585/mmwr.mm6722a1
- Symptoms of PTSD. (n.d.). Anxiety and Depression Association of America, ADAA. https://adaa.org/understanding-anxiety/posttraumatic-stress-disorder-ptsd/symptoms
- Tighe, J., Nicholas, J., Shand, F., & Christensen, H. (2018). Efficacy of acceptance and commitment therapy in reducing suicidal ideation and deliberate self-harm: Systematic review (Preprint). https://doi.org/10.2196/preprints.10732
- Why more men are taking their own lives. (n.d.). Verywell Mind. https://www.verywellmind.com/men-and-suicide-2328492
- Zhong, Q., Gelaye, B., Fricchione, G. L., Avillach, P., Karlson, E. W., & Williams, M. A. (2018). Adverse obstetric and neonatal outcomes complicated by psychosis among pregnant women in the United States. BMC Pregnancy and Childbirth, 18(1). https://doi.org/10.1186/s12884-018-1750-0
To access Fast Facts, purchase this course or a Full Access Pass.
If you already have an account, please sign in here.
To access Fast Facts, purchase this course or a Full Access Pass.
If you already have an account, please sign in here.

